In this episode, we delve into the often overlooked but vital organ, the liver. We explore the liver's location, size, and its myriad of functions, which go far beyond detoxification to include digestion, metabolism, blood sugar regulation, and maintaining a healthy gut microbiome. The episode highlights the challenges to liver health posed by modern lifestyle choices, including exposure to toxins, chemicals, and the overuse of medications.
Read more...
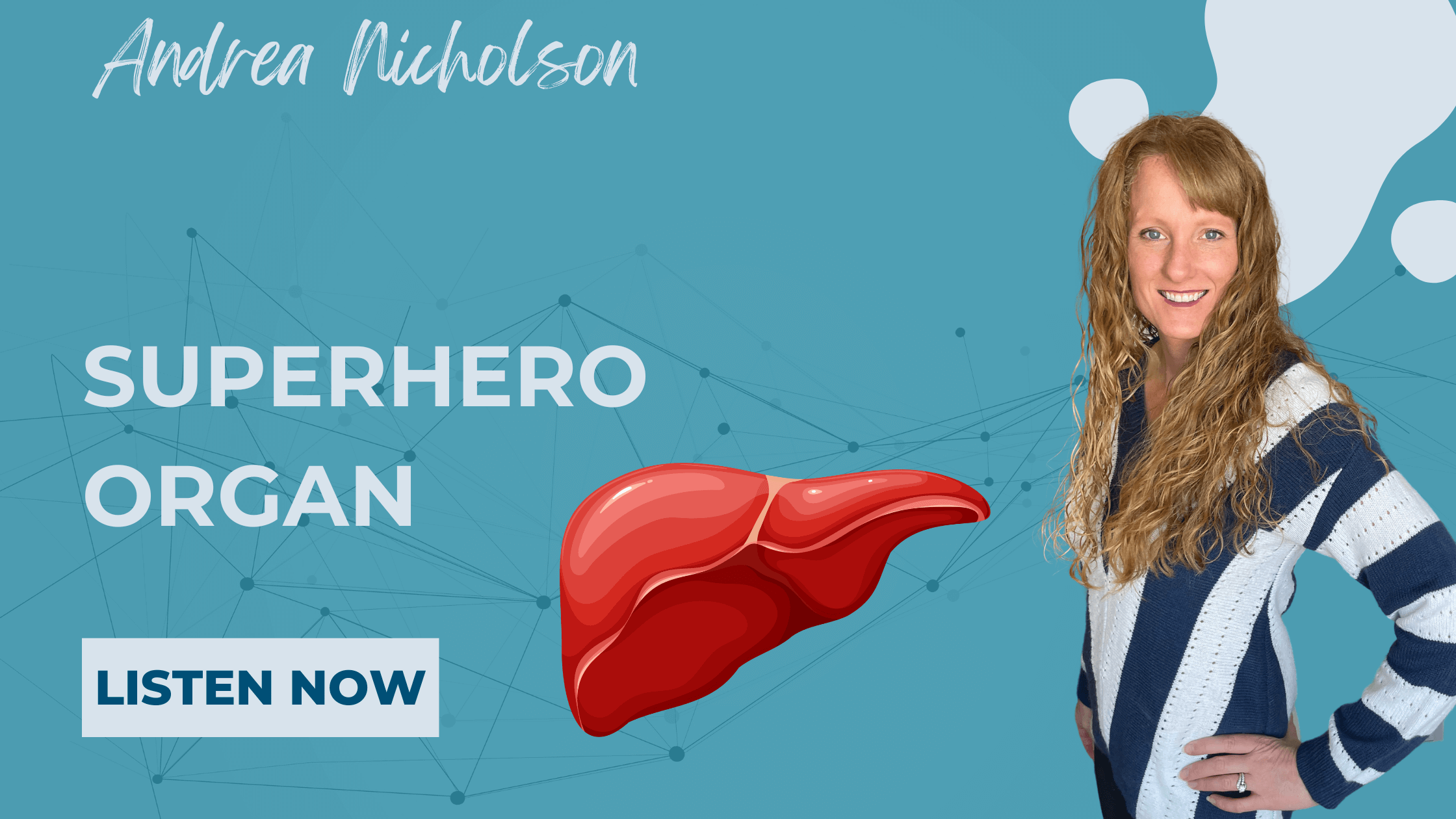
Your gut and brain are closely connected, and inflammation might harm both. A weakened blood-brain barrier (leaky brain) lets harmful substances into the brain, potentially leading to mental health issues like depression and neurodegenerative diseases. This is similar to leaky gut, where a loose intestinal lining allows toxins into the bloodstream.
Research shows that improving gut health—through probiotics, prebiotics, a healthy diet, and lifestyle changes—can strengthen the gut-brain connection and reduce inflammation. Addressing gut health could be a key step in improving mental health and preventing brain-related conditions.