Could this nutrition therapy be an answer for people with type 2 diabetes and obesity? Protein Sparing Modified Fasting is a fast from carbohydrates and most fat, focusing entirely on protein. This particular study examined the effects of this type of nutrition plan for 7 adults with long standing type 2 diabetes and obesity.
Looking for a natural approach to solving your health challenges? Apply to work with me.
Read the study: https://diabetesjournals.org/diabetes/article/25/6/494/4083/Nitrogen-Metabolism-and-Insulin-Requirements-in
EPISODE DETAILS:
Welcome back to the Holistic Health Bites podcast where we discuss all things metabolic health. Today, we're discussing a powerful study published in the journal Diabetes on a unique approach to managing obesity and type 2 diabetes.
This particular study evaluated the effectiveness of a nutrition therapy known as protein sparing modified fasting.
The first interesting tidbit was this study was published in 1976! So, this is NOT new information. Sadly, it has not been widely utilized in the era of modern medicine. But stick with me, because this research still holds valuable insights today.
Fasting has long been used as a natural way to lose weight, fat, reduce blood sugar and insulin, as well as for many medical procedures. It’s not inherently dangerous, when done properly, but it can be difficult for some people to fully eliminate all foods and beverages other than water. And, most of us can only fully fast for so long before nutrient deficiencies set in. Protein sparing modified fasting is fasting from carbs and most fat, but still provides nutrients in the form of protein - specifically in this study egg whites and lean beef.
The researchers looked at seven obese adults with type 2 diabetes who were taking on insulin. These patients were put on a special diet that included:
- 1.2 to 1.4 grams of protein per kilogram of their ideal body weight
- As much water as they wanted
- Vitamin and mineral supplements
And that's it. No carbs, no fats - just protein, water, and vitamins.
Let’s run through each patient in this study:
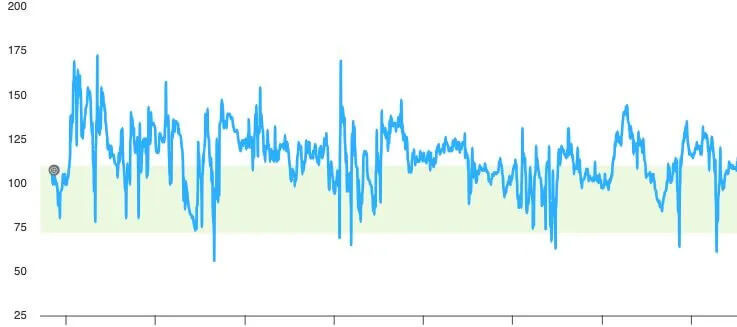
Patient 1: 47 year old female who had been morbid obese most of her life and had been diagnosed with type 2 diabetes 11 years prior. She weighed 334 lbs, 5’10” tall, and was taking about 52 units of insulin daily. On this plan, she was given 150g of protein per day and her insulin was progressively reduced from 40 units the first 3 days, then 20 units for 4 days, then 10 units for 11 days, then by day 18 no insulin was needed. She was also down about 25lbs. In 1 year she lost 162 lbs.
Patient 2: 63 year old female with obesity for over 40 years, had been diagnosed with diabetes 6 years prior, also had history of cardiac arrest. She was on 100 units of insulin at the outset of the study, weighed 214 lbs, 5’ tall. At the beginning of the study, she was given 75g protein with 25g carbohydrates for the first 5 days, then insulin was reduced to a total of 80 units, then 40 units after 9 days, then discontinued after 10 more days. She lost 15 lbs in the first 3 weeks. She ultimately wasn’t compliant with the PSMF plan, so she required some oral diabetes medications. Three months in, she weighed 182lbs (down 32 lbs). Protein dose was decreased to 65g which brought her glucose down to normal ranges within 3 days. She stopped the oral medication after 6 days. At the one year mark, despite not being fully compliant with the diet, she weighed 138 lbs with only slightly elevated blood glucose levels (109).
Patient 3: 60 year old female, obese for 34 years, had been diagnosed with type 2 diabetes 11 years prior and subsequently suffered a transient drug-induced kidney failure episode which caused her to need insulin. She was on 55 units of insulin which was poorly controlling her glucose levels. She had multiple other conditions including heart disease, gout, prior heart attack, hypothyroidism, and had previously had a hysterectomy and gallbladder removed. She weighed 226lbs at 5’3” tall. She began PSMF at 99g of protein daily and her insulin was stopped simultaneously. After 15 days, she was down 6.6 lbs. At 10 months, she was down 83.6 lbs.
Patient 4: 55 year old male with mild obesity and a colostomy after an abdominal gunshot wound. He’d been diagnosed with diabetes 5 years prior, requiring insulin at 30 units per day. He also had severe hypertension, heart disease and gout. He started at a weight of 275 lbs, 5’11” tall. He began with 125g of protein daily and his insulin was reduced to 20 units per day, then discontinued after 4 days. In 18 days, he was down 22 lbs and had reduced his blood pressure medication. At home, he was not compliant with the diet, and regained 11 lbs in 10 weeks, and returned to 20 units of insulin. When back on the diet for a needed surgery related to the colostomy, at 120g protein daily, off of insulin, he lost 41.8 lbs in 6 weeks. Following surgery, he again, fell off with compliance, regained to 207 lbs and needed insulin again.
Patient 5: 49 year old female, obese since childhood and had been diagnosed with diabetes 8 years prior. She was on 10 regular units of insulin and 90 units of intermediate insulin daily. She also had peripheral neuropathy, hypertension, and high cholesterol. She weighed 206 lbs at 5’5” tall. She started off with 73g of protein daily, with steadily decreasing intermediate insulin doses, and her hypertension medication was stopped. After 4 months, she was down 39.6 lbs, off all insulin and maintained the loss for the following 6 months.
Patient 6: 60 year old female, obese since childhood, had been diagnosed with diabetes 23 years prior. She was currently on 25-30 units of intermediate insulin daily. She had hypertension, gallbladder removed, hepatitis, and prior heart attack. She began at 156 lbs at 5’1” tall. She began at 80g of protein per day, insulin and hypertension medications were stopped. At 2 months, she had lost nearly 20 lbs and regained less than 1 lb over the following 5 months.
Patient 7: 52 year old male, obese since early adulthood, had been diagnosed with diabetes 15 years prior. He was initially on 40 units intermediate insulin and 20 units of regular insulin daily. He also had history of kidney stones, kidney inflammation, COPD, prostate cancer, and hernias after gallbladder removal. He started at 250 lbs at 5’7” tall. He began with 110g of protein per day, reducing insulin by 50% initially, then discontinuing after 1 week. In 4 months, he was down 46 lbs. He was not compliant with the diet, taking in more protein than prescribed, causing blood sugar spikes and the need for insulin to return at 10-15 units of intermediate acting per day. At 13 months, he as back to his original weight.
In the end, this diet had some pretty remarkable effects:
- It controlled both carbohydrate metabolism and hunger.
- It reduced blood sugar and insulin levels.
- It increased the levels ketone bodies in the blood.
- And helped them get off of medications including insulin, oral diabetes and hypertension on average in just 6.5 days.
Now, you might be wondering - isn't this just another crash diet that'll wreck your muscle mass? Well, that's the truly fascinating part. The researchers found that patients could maintain their nitrogen balance - a key indicator of preserving muscle mass - on this diet.
Of course, this was a small study conducted many years ago, but it raises some intriguing questions about how we approach weight loss and diabetes management. Could a high-protein, low fat and low carb nutrition plan be a useful tool for some patients? It absolutely is an option.
I personally, don’t consider this to be a long term strategy as described, but I do strongly believe that this can be a tool in the toolbox to make significant changes in your health, as can a well formulated ketogenic, low carb or carnivore plan. My main concern with the PSMF long term is dropping too much body fat. Body fat really isn’t the enemy, as it is essential to health. We don’t want too much, we don’t want fat in the wrong places like surrounding our organs, but we also don’t want to be too lean. Fat is active tissue that serves many purposes throughout the body. Many of the current proponents of this style of eating are excessively thin, which likely will bring long term consequences.
They did note that when the protein intake got too low, nitrogen balance was not maintained, which would indicate muscle/lean tissue loss. And when protein was too high in those with type 2 diabetes, blood sugar levels increased requiring medications. The perfect protein amount likely will vary greatly for each person based on their unique metabolism and health status.
As always, it is recommended that you work with your healthcare team or an expert on this type of nutrition therapy to ensure safety, especially when it comes to modifying medications. These types of diets can be so effective so quickly, that overmedication can be a serious risk - and life threatening at that.


















0 Comments